Advanced BMI Calculator: Age-Adjusted Weight & Health Metrics
Free BMI Calculator 2026 to calculate your Body Mass Index and check your healthy weight range with accurate BMI categories and chart.
Enter Your Details
Health & Fitness Calculators
Track your health and fitness goals.
BMI Table for Adults
The following classification system for adults aged 20 and older follows recommendations established by the World Health Organization (WHO). This standardized approach applies uniformly to both men and women. The BMI ranges provide a consistent framework for health assessment across different populations.
| Classification | BMI Range (kg/m²) |
|---|---|
| Severe Thinness | < 16 |
| Moderate Thinness | 16 – 17 |
| Mild Thinness | 17 – 18.5 |
| Normal Weight | 18.5 – 25 |
| Overweight | 25 – 30 |
| Obese Class I | 30 – 35 |
| Obese Class II | 35 – 40 |
| Obese Class III | > 40 |
BMI Chart for Adults
A visual representation of adult BMI categories helps illustrate how different weight ranges relate to overall health classification. Reference data from the World Health Organization establishes these boundaries to help individuals understand where their BMI falls within the health spectrum. The chart shows clear demarcation lines between each category, with the normal weight range (18.5–25) positioned in the center as the reference standard for adult health assessment.
BMI Table for Children and Teens (Ages 2–20)
Interpreting BMI in children and adolescents differs fundamentally from adult assessment because growing bodies change in different ways at different ages. The Centers for Disease Control and Prevention (CDC) uses percentile-based BMI-for-age standards that account for age and biological sex. This approach recognizes that healthy BMI ranges shift as children mature, ensuring more accurate health classification during developmental years.
| Category | Percentile Range |
|---|---|
| Underweight | < 5% |
| Healthy Weight | 5% – 85% |
| At Risk of Overweight | 85% – 95% |
| Overweight | > 95% |
BMI Chart for Children and Teens (Ages 2–20)
Growth charts developed by the CDC present BMI assessment through a percentile-based framework specific to age and biological sex. Separate charts for boys and girls reflect natural developmental differences that occur during childhood and adolescence. The percentile approach allows medical professionals and caregivers to compare an individual child's BMI against age-matched peers, providing context that straight numerical values alone cannot supply during rapid growth phases.
Risks Associated with Being Overweight
A higher BMI may correlate with increased health risks across multiple physiological systems. Health organizations including the CDC have documented connections between elevated BMI and various chronic conditions. While BMI alone does not diagnose disease, it serves as a useful screening indicator that warrants further medical discussion, particularly when combined with other health markers.
- •Elevated blood pressure and cardiovascular strain
- •Type 2 diabetes and glucose regulation complications
- •Heart disease, stroke, and atherosclerosis progression
- •Joint deterioration and reduced mobility
- •Sleep apnea and breathing difficulties
- •Increased susceptibility to certain cancers
- •Reduced quality of life and mental health considerations
These associations underscore the importance of consulting with qualified healthcare professionals for personalized health guidance and risk assessment.
Risks Associated with Being Underweight
Low BMI may indicate nutritional insufficiency or underlying health concerns that require medical attention. Being significantly underweight can compromise multiple body systems and increase vulnerability to various health complications.
- •Nutritional deficiencies including iron, vitamin B12, and folate
- •Weakened bone density and increased fracture risk
- •Hormonal imbalances and reproductive health concerns
- •Compromised immune system function
- •Increased surgical and anesthetic risk
If you fall significantly below normal BMI range, medical evaluation is recommended to identify and address underlying causes.
Limitations of BMI
BMI serves as a convenient screening metric but has important limitations that healthcare providers recognize. The calculation does not differentiate between muscle mass, bone density, and fat distribution. An athlete with significant muscle development may show a higher BMI despite lower body fat percentage. Genetic factors, age-related changes, and individual metabolic variations all affect how BMI relates to actual health status. Therefore, BMI should never be used in isolation as a diagnostic tool and is best interpreted alongside other health measurements and clinical assessment.
BMI in Adults
In adult populations, BMI functions as a practical population-level screening mechanism rather than an individual diagnostic instrument. Healthcare systems employ BMI as an initial assessment filter to identify individuals who may benefit from more comprehensive health evaluation. It helps organize larger populations for epidemiological research and public health initiatives. However, individual adults should understand that their personal BMI number is just one data point in a comprehensive health profile. Factors such as muscle composition, cardiovascular fitness, metabolic markers, and family history all contribute to overall health assessment alongside BMI.
BMI in Children and Adolescents
Pediatric BMI interpretation requires special consideration because children are constantly growing and changing body composition. Growth spurts, hormonal fluctuations, and developmental variations mean that a child's weight-to-height relationship changes substantially from infancy through adulthood. Percentile-based assessment accounts for these natural developmental patterns by comparing each child against age and sex-specific reference data. This percentile approach prevents misclassification that would occur if adult BMI categories were applied directly to growing children. Parents and pediatricians should work together to monitor growth trends over time rather than focusing on any single BMI measurement.
BMI Prime
BMI Prime expresses an individual's BMI as a ratio compared to the upper boundary of the normal healthy range (25 kg/m²). This comparative measurement simplifies cross-population comparison by converting absolute BMI values into proportional terms. A BMI Prime of 1.0 indicates BMI exactly at the upper normal limit, while 1.2 means BMI is 20% above that threshold. This standardization method can help individuals quickly grasp how their BMI relates to standard health guidelines without memorizing all the categorical boundaries.
| Classification | BMI Range | BMI Prime |
|---|---|---|
| Severe Thinness | < 16 | < 0.64 |
| Moderate Thinness | 16 – 17 | 0.64 – 0.68 |
| Mild Thinness | 17 – 18.5 | 0.68 – 0.74 |
| Normal Weight | 18.5 – 25 | 0.74 – 1 |
| Overweight | 25 – 30 | 1 – 1.2 |
| Obese Class I | 30 – 35 | 1.2 – 1.4 |
| Obese Class II | 35 – 40 | 1.4 – 1.6 |
| Obese Class III | > 40 | > 1.6 |
BMI Prime offers a normalized comparison method that simplifies understanding of where any given BMI sits relative to standard health thresholds, making it useful for tracking personal progress or comparing across different age groups.
Path to Improved Health
Improving your health is a gradual journey that extends well beyond any single metric. Long-term wellbeing depends on consistent physical activity, thoughtful nutrition choices, and developing mindful habits. These foundational practices work together to support sustainable health improvements and increased energy levels throughout daily life.
Exercise Regularly
Regular physical activity strengthens your cardiovascular system, builds and preserves muscle tissue, and enhances metabolic function. Consistent movement—whether walking, jogging, or stretching—contributes to improved circulation, better sleep quality, and increased overall vitality. The key to lasting results is finding activities you enjoy and maintaining a sustainable routine rather than pursuing intense efforts sporadically.

Eat Healthy Food
A balanced diet incorporating fruits, vegetables, whole grains, and lean proteins provides essential nutrients your body needs for optimal function. Mindful portion awareness and choosing nutrient-dense foods over heavily processed options helps maintain steady energy levels. Avoiding extreme dietary restrictions allows for sustainable eating patterns that you can maintain long-term without frustration or deprivation.

Avoid Overeating
Mindful eating practices help distinguish true hunger from other triggers like stress or boredom. Eating regular meals at consistent times stabilizes blood sugar and reduces the likelihood of excessive consumption. Paying attention to fullness cues and eating without significant distractions supports more balanced nutrition and greater awareness of your body's actual needs.
Alternate Estimates of Weight-Related Health Risks
BMI provides a general screening foundation but captures only one dimension of health risk. Body fat distribution, where excess weight concentrates on your body, may carry different health implications than BMI alone suggests. Additional measurements can complement BMI assessment and offer insights into metabolic health and cardiovascular risk factors.
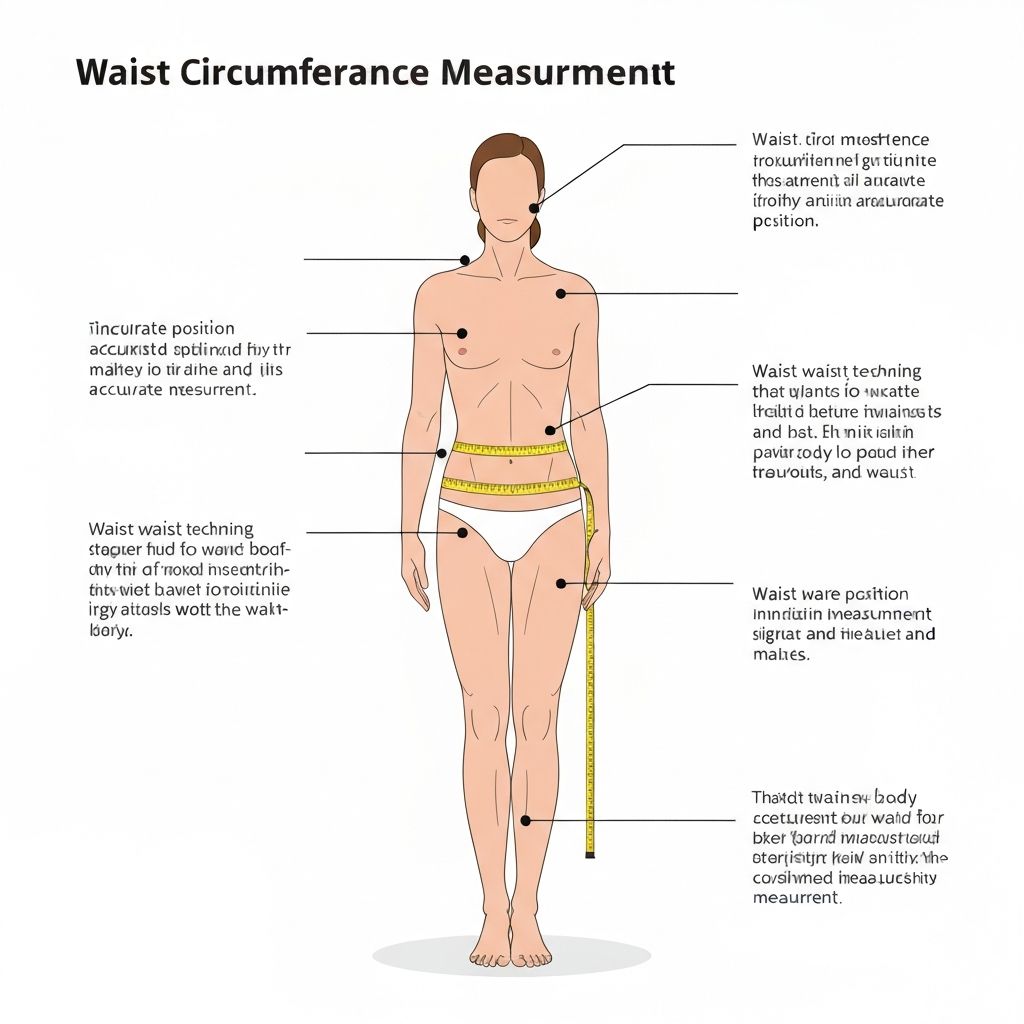
Waist Circumference
Waist circumference measures abdominal fat distribution, which correlates with visceral fat accumulation around organs. Excess abdominal fat has distinct metabolic consequences compared to fat stored in other locations. This measurement complements rather than replaces BMI, providing additional context for understanding individual health risk profiles and patterns associated with chronic disease.
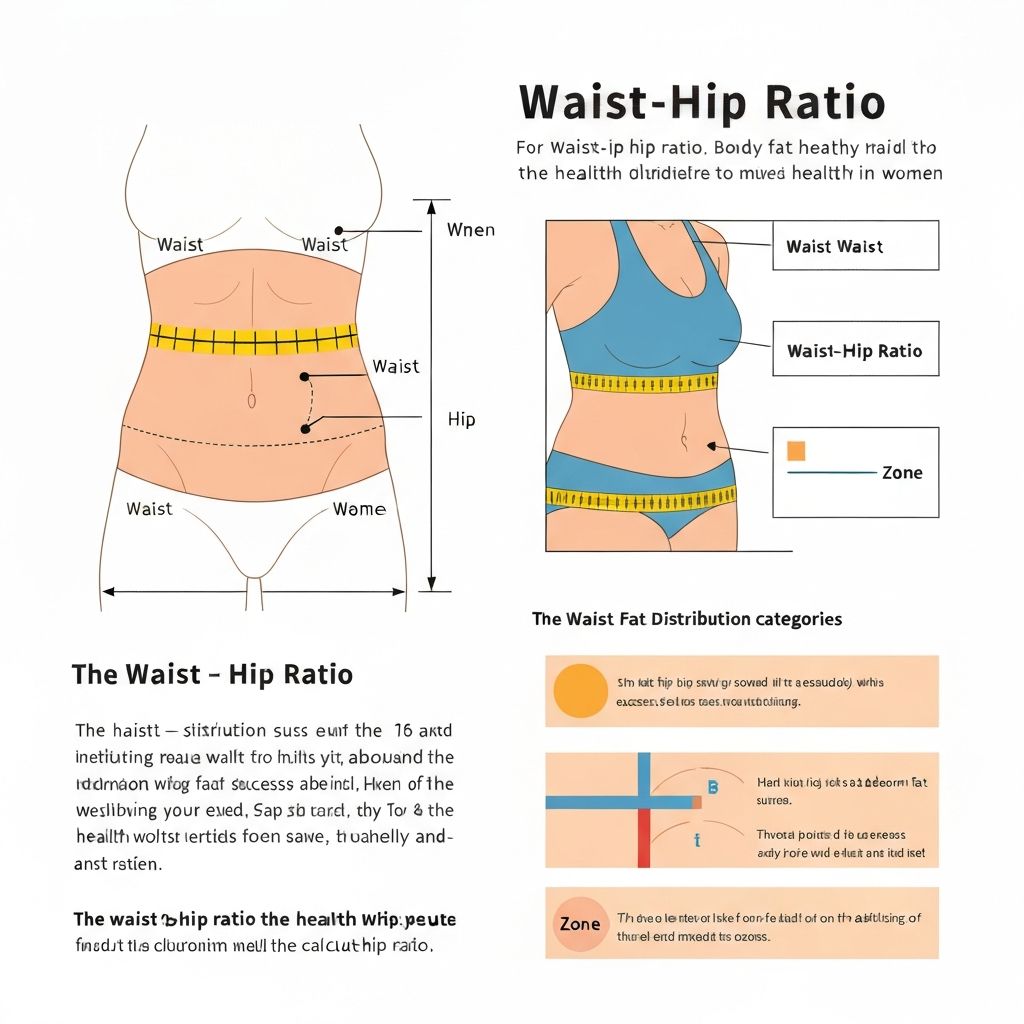
Waist-to-Hip Ratio
Comparing waist measurement to hip measurement reveals how weight distributes across your body. Fat accumulation in the abdomen (apple-shaped distribution) carries different health implications than fat concentrated in hips and thighs (pear-shaped distribution). This ratio offers a perspective on body fat distribution patterns that influences health risk assessments and metabolic considerations.
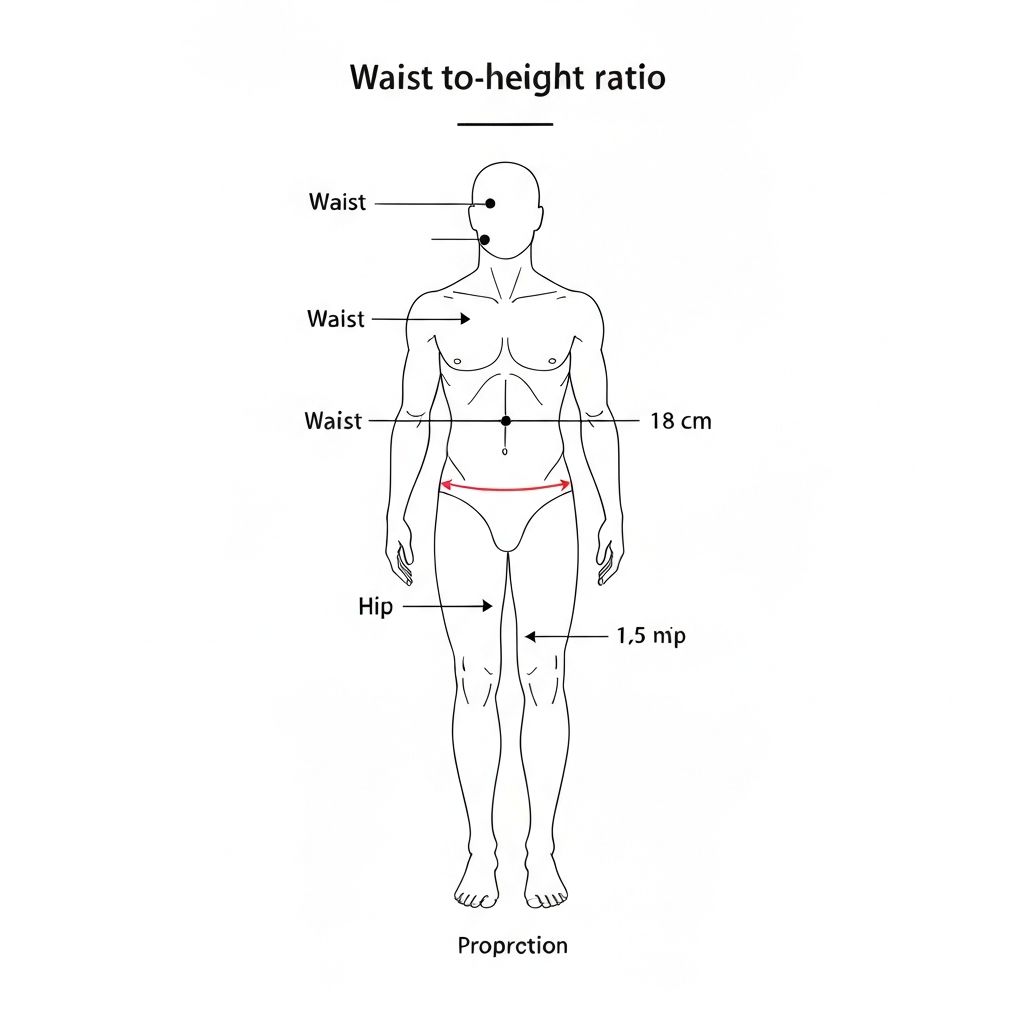
Waist-to-Height Ratio
This ratio evaluates abdominal fat relative to total body height, accounting for individual height variations that BMI already includes. Some research suggests waist-to-height ratio may indicate metabolic health risk across diverse populations. Like other alternative measurements, it works best when considered alongside BMI and other health markers rather than as a standalone assessment tool.
Important Medical Note
BMI may overestimate body fat in muscular or athletic individuals and may not accurately reflect body composition for children, elderly, pregnant women, or people with certain medical conditions. Always consult a healthcare provider for personalized health assessment.
Trust & Transparency
Reviewed & Maintained By:
VIP Calculator Research Team
Methodology:
Uses internationally recognized BMI, Ponderal Index, and Body Surface Area formulas referenced in academic and health literature
Purpose:
Educational and informational use only
Limitations:
May not be accurate for athletes, children, or during pregnancy
Privacy:
All calculations run locally in the browser; no personal data is stored or transmitted
📖 How to Use the BMI Calculator
- Enter your weight in kilograms or pounds
- Enter your height in centimeters, meters, or feet and inches
- Optionally add age and waist circumference for advanced metrics
- Click Calculate to see your BMI result and health analysis
🔢 BMI Calculation Formula
Body Mass Index is calculated using your weight and height.
BMI = weight (kg) / height² (m²)
Or: BMI = (weight (lbs) / height² (inches²)) × 703
✨ Key Features of the BMI Calculator
- Calculate BMI using metric or imperial units
- Instant BMI category classification with WHO standards
- Interactive weight position slider with real-time updates
- Healthy weight range calculator with min/max targets
- Age-specific BMI context for children and teenagers
- Advanced health metrics: Ponderal Index, BSA, WHtR
- Step-by-step calculation breakdown
- Athletic disclaimer for muscular individuals
- Personalized health recommendations
🎯 Benefits of Using the BMI Calculator
- Professional health assessment tool with medical accuracy
- Monitor weight management progress over time
- Understand your healthy weight range instantly
- Better predictor with Waist-to-Height Ratio
- Set realistic fitness goals based on data
- Age-appropriate BMI interpretation
- Free alternative to basic doctor screenings
❓ Frequently Asked Questions
What is a healthy BMI range?
A healthy BMI typically falls between 18.5 and 24.9 for adults. However, BMI is just one indicator of health and should be considered alongside other factors like waist circumference and body composition.
Is BMI accurate for bodybuilders?
No, BMI is not accurate for bodybuilders or very muscular individuals. BMI doesn't distinguish between muscle and fat mass, so athletes may be classified as overweight despite having low body fat. Use body fat percentage or waist-to-height ratio instead.
What is a dangerous BMI level?
A BMI below 16 (severely underweight) or above 40 (Class III obesity) is considered dangerous and requires immediate medical attention. BMI below 18.5 or above 30 also poses health risks and should be discussed with a healthcare provider.
Can children use this BMI calculator?
This calculator shows adult BMI ranges, but if you enter an age under 20, it will display a note explaining that children and teens require age and gender-specific BMI percentile calculations. Please consult a pediatrician for accurate child/teen BMI assessment.